
Correlation between Fecal Incontinence and Pressure Injury
Correlation between Fecal Incontinence and Pressure Injuries
Fecal incontinence affects all spans of life including children, men, and women of all ages, however, it is most prevalently seen in the population over 65 years old, affecting approximately 2.2% of the demographic.
It is also found that patients with fecal incontinence were 22 times more likely to have pressure injuries than patients without fecal incontinence.¹
Types of Fecal Incontinence
Fecal incontinence is the inability to control bowel movements, causing stool to leak unexpectedly from the rectum. A decrease in quality of life was also noted in those with fecal incontinence.
Types of fecal incontinence include:
- Anal Incontinence – involuntary loss of feces, flatus, and/or mucus, the broadest type compared to the other types of bowel incontinence.
- Flatus bowel incontinence – the sensation of a full rectum, but unable to decipher between stool or flatus leading to unexpected accidents.
- Mucus incontinence – bowel leaks due to being too full. This can be due to a loss of feeling in your lower abdomen/perineal area or difficulty in emptying your bowels effectively.
- Fecal incontinence – involuntary loss of feces.²
Causes and Risk Factors for Fecal Incontinence
Causes of fecal incontinence can include factors such as old age, frequent diarrhea, and constipation. These conditions cause the muscles in the rectum and anus to weaken. When these muscles weaken, the ability to hold stool within the body also weakens. Muscles in the rectum and anus also naturally weaken with age.
Risk factors for fecal incontinence can include³:
- Muscle Damage
- Pelvic Organ Descent and Prolapse
- Central Nervous System
- Damage to the Nerves
- Inability of the Rectum to Stretch
- Laxative Abuse
- Radiation Treatments
- Spina Bifida and more
Fecal Incontinence and Skin Integrity
Normal feces is alkaline, with a typical pH of 7.0 to 7.5, contributing to an abnormal skin pH in incontinent patients.
Incontinence damages the tissue integrity of the skin, which leaves patients susceptible to skin breakdown, such as pressure injuries and incontinence-associated dermatitis (IAD). Fecal enzymes in the presence of ammonia cause skin erosions.
Once the skin has broken down, it will never be as strong or resilient as it once was. It’s estimated that patients only acquire 80% of their skin’s strength back once healed.⁴
Incontinence Associated Dermatitis
Incontinence-associated dermatitis (IAD) is an inflammation of the skin that may occur when urine or stool comes into contact with perineal or perianal skin.⁵ Incontinence and IAD are both independent risk factors for higher-stage pressure injuries.
IAD is characterized by inflammation and/or erosion of the skin associated with exposure to urine or stool. Studies at long-term care facilities show IAD prevalence can range from 5.6% to 50%, while incidence rates range from 3.4% to 25%. Among incontinent patients, the prevalence of IAD ranges from 18% to 45.7% The prevalence of IAD for incontinent patients affects 11% of the general patient population.⁶
Fecal Incontinence and Risk of Pressure Injury
There is a prevalent correlation between fecal incontinence and pressure injuries. Patients with fecal incontinence were 22 times more likely to have pressure injuries than patients without fecal incontinence, and there is a higher risk of skin breakdown and incontinence in older patients, particularly those over the age of 80.
Additionally, the odds of having a pressure ulcer (injury) were 37.5 times greater in patients who had both impaired mobility and fecal incontinence than in patients who had neither.⁷
Pressure Injury vs Incontinence Associated Dermatitis (IAD)
A pressure injury (also called a bedsore, pressure ulcer, pressure sore, or decubitus ulcer) is an area of injured skin.⁸ It has both similarities and differences to Associated Dermatitis.⁹
| Pressure Injury | Associated Dermatitis |
| Located over bony prominences – coccyx, tailbone or ischia (butt bones) | Location is where the skin lays in or on urine or feces, not only over a bony prominence |
| Usually round or oval shaped | Early injury is bright red and can be weepy |
| Over sacrum may be butterfly shaped or oval if mostly on one side | Post-acute skin is purplish and very dry, peeling like a sunburn |
| Well-defined edges – no satellite lesions | No satellite lesions |
Pressure Injury Treatment Options
Treatment of pressure injuries often requires a multidisciplinary approach involving nurses, physicians, and other members of a care team.
Treatment interventions include:
- Management of conditions that give rise to pressure injuries (support surfaces and nutritional support)
- Protection and promotion of wound healing (wound dressings; topical applications; and various adjunctive therapies that are used in addition to standard pressure injury care, such as vacuum-assisted closure, ultrasound therapy, electrical stimulation, and hyperbaric oxygen therapy)
- Surgical repair of the wound.¹⁰
The use of Alocane® Plus can also help relieve the pain and itch associated with early-stage pressure injuries.
Alocane® Plus
Alocane® Plus is a topical gel containing 4% lidocaine (a topical analgesic) and 0.13% benzalkonium chloride (a topical antiseptic), along with other skin care ingredients such as aloe and vitamin E. This product may be useful for the temporary treatment of pain and preventing infection in early-stage pressure injuries.
In an observational study, topical lidocaine was associated with significant reductions in pain intensity in patients with a variety of painful wounds, including pressure injury. An additional retrospective study found that topical application of 4% lidocaine was safe and effective for temporarily reducing pain during the debridement of digital ulcers secondary to systemic sclerosis.
Benzalkonium chloride has been shown to decrease bacterial biofilm burden in vitro studies and murine wound models. Therefore, it may be useful to prevent infection or biofilm formation in patients with pressure injuries. The “inactive” ingredients aloe and vitamin E have additional properties that may be beneficial to wound healing.
Establishing a Bowel Care Program for Fecal Incontinence
Fecal incontinence is a treatable condition that, if prevented, can also aid in the prevention of pressure injuries. The goals of establishing a bowl care program for fecal incontinence include:
- Improve stool consistency
- Establish a regular time for elimination
- Initiate complete rectosigmoid emptying on a regular basis
ENEMEEZ® mini enemas can be an effective part of a bowl care program to reduce the incidence of fecal incontinence.
ENEMEEZ® Mini Enemas
The ENEMEEZ® formulation acts as a hyperosmotic, stool-softening laxative that works by drawing water into the bowel from surrounding body tissues used to treat general constipation and incontinence. The docusate sodium in this mini enema product prepares the stool to readily mix with watery fluids. It softens and loosens stool and initiates a normal, replicated bowel movement, typically within 2-15 minutes.
ENEMEEZ® Plus is the same formulation as ENEMEEZ®, with the addition of 20mg of benzocaine, assisting in the anesthetization of the rectum and lower bowel. This formulation was developed for patients who experience autonomic dysreflexia, hemorrhoids, anal fissures, or painful bowel movements.
ENEMEEZ® Versus Competing Products
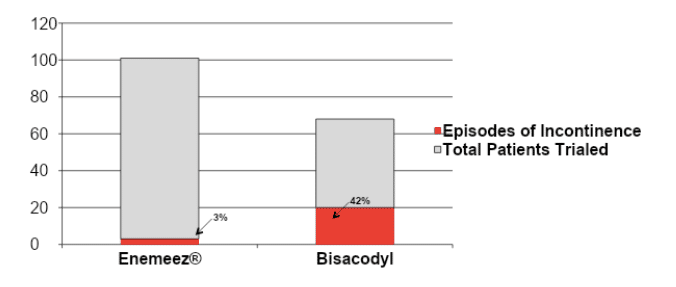
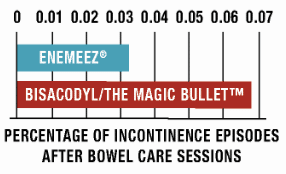
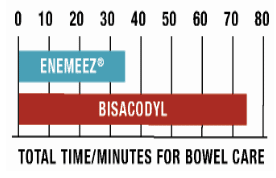
In a case study¹¹ ENEMEEZ® mini-enema users had less than half of the incontinence episodes as compared to the competitor using Bisacodyl and provided an evacuation in 35 minutes compared to 75 minutes with the competing product. 42% of Bisacodyl users experienced at least one episode of incontinence when using a suppository, whereas that number drops significantly, to only 3%, when using ENEMEEZ® mini-enemas.
Request ENEMEEZ® mini enemas or Alocane® Plus samples for your patients today.
Request an Educational In-Service
Are you interested in learning more about this topic, among others, and educating those within your healthcare facility? Request a virtual 20-30 minute Educational In-Service for your team today, and we’ll even have lunch delivered to your office!
Disclaimer: The material contained is for reference purposes only. Quest Healthcare, A Division of Quest Products, LLC, does not assume responsibility for patient care. Consult a physician prior to use. Copyright 2022 Quest Healthcare, A Division of Quest Products, LLC.
Sources:
- Brown HW, Wexner SD, Segall MM, Brezoczky KL, Lukacz ES. Accidental bowel leakage in the mature women’s health study: prevalence and predictors. Int J Clin Pract. 2012;66(11):1101–8.
- Bliss DZ, Johnson S, Savik K, Clabots CR, Gerding DN. Fecal incontinence in hospitalized patients who are acutely ill. Nurs Res. 2000;49(2):101–8.
- https://my.clevelandclinic.org/health/diseases/14574-fecal-bowel-incontinence
- Driver, D. (2007). Perineal dermatitis in critical care patients. American Association of Critical Care Nurses, 27, 42-46.
- Gray M, et al., J Wound Ostomy Continence Nurs. 2007 Jan-Feb;34(1):45-54.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8601665/pdf/wocn-48-545.pdf
- Maklebust J, Magnan MA, Adv Wound Care. Nov 1994;7(6):25, 27-8, 31-4 passim, 2. J. Wound Ostomy Continence Nurs. 2008; 35 (1): 104-110.
- https://my.clevelandclinic.org/health/diseases/17823-pressure-injuries-bedsores
- https://omniamedsso.om-systems.net/sso/check_site_login/site_id/15/login_type/2/ip_hash/128c3e1763ce9affd8f695afc832d406#:~:text=Differentiating%20between%20IAD%20and%20pressure%20injury&text=IAD%20is%20a%20’top%20down,injury%20(Figure%201)17.
- https://www.acpjournals.org/doi/10.7326/m14-1568#r1-10
- Case Study: Glen House, J, & Stiens, S. Pharmacologically initiated defecation for persons with spinal cord injury: effectiveness of three agents. Arch Phys Med Rehabil, 78, 1062-106







